On October 11th, 2021, pharmaceutical company Merck submitted an Emergency Use Authorization (EUA) application to the US Food and Drug Administration (FDA) for a COVID-19 treatment pill. On Tuesday November 16th, 2021, Pfizer engaged in the identical process of seeking FDA approval for a pill intended to meet the same purpose.
Both of these pills involve curing individuals who have been recently diagnosed with COVID-19. The objectives of the pills are not to be mistaken with the COVID-19 vaccines, as the vaccines focus upon ensuring protection from the virus, whereas the intentions of the Merck and Pfizer pills are to solely aid in curing people who have been diagnosed. While the two companies hope to achieve approval by the same administration, several differences are evident concerning the pills’ efficacy rates, risks and benefits, how they work, etc.

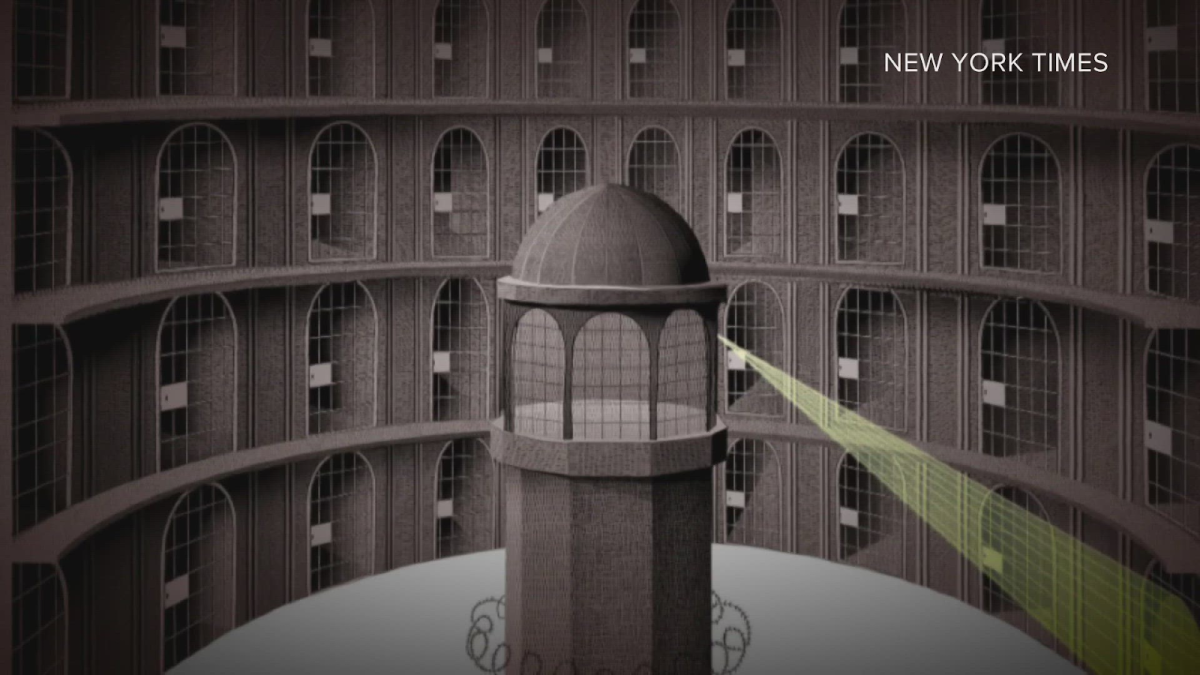
In regards to the Merck pill, while the FDA has yet to authorize the antiviral COVID-19 pill, it has in fact been approved by the EU (European Union) regulatory system, the European Medicine Agency (EMA). Some of these countries include France, Germany, Greece, Italy, and Spain. The pill called molnupiravir, named after Mjölnir, the hammer of Thor, has an efficacy rate of 50% for death and hospitalizations, and pertains to patients who begin treatment within five days. After someone takes molnupiravir, the drug is transformed into something similar to a RNA chemical building block. “The modification is so subtle that not only will the coronavirus use molnupiravir in place of other building blocks when it replicates itself, but coronaviruses’ unusual proofreading mechanism can’t even pick up on the imposter compound. Over time, the drug will encourage the virus to introduce even more mistakes” (STAT). This introduces numerous differentiating mutations which allows for nothing further to happen. The study demonstrated results where none of almost four hundred patients that received the Merck pill in the trial died (The New Yorker).
Likewise, the FDA has not yet approved of Pfizer’s recently fabricated pill, named Paxlovid. However, differences lie in the efficacy rates, as this pill remains 89% effective with reference to the risk of death or hospitalization (The New York Times). It has been stated, “In the overall study population through Day 28, no deaths were reported in patients who received PAXLOVID™ as compared to 10 deaths in patients who received placebo” (Pfizer). The study was submitted for approval to the FDA on November 9th, not long ago. Dissimilarities may additionally be seen through how the pill works in comparison to molnupiravir. Paxlovid allows for the strings of RNA to be assembled correctly to make viral proteins, which are originally produced in a chunk. The Pfizer drug binds a point in an enzyme which divides proteins. Essentially, the virus would not be able to recreate usable copies without the point in the enzyme.
While the pill from each pharmaceutical company works differently, their intentions remain the same—developing a treatment for people infected with COVID-19.